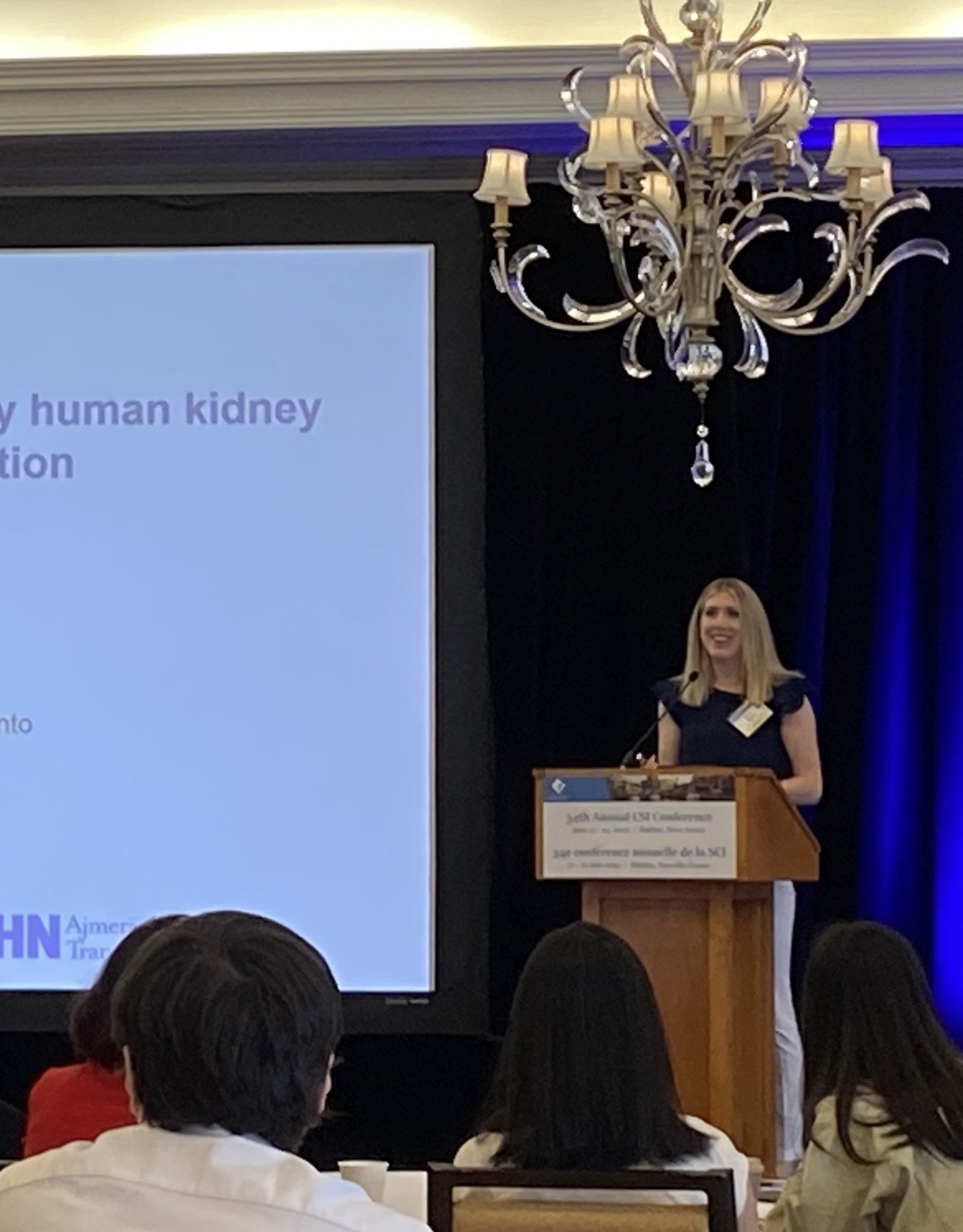
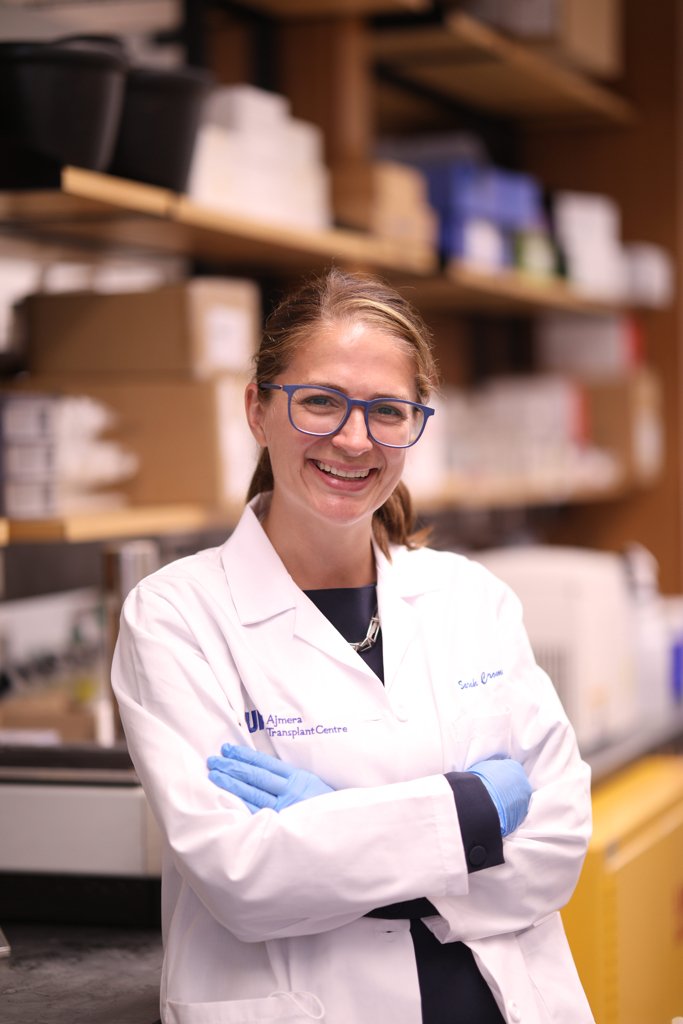
Sarah Crome, PhD Assistant Professor | University of Toronto | Faculty of Medicine | Department of Immunology Scientist | University Health Network | Toronto General Hospital Research Institute | Multi Organ Transplant Medicine by Design Investigator
Dr. Sarah Crome was recruited to the University of Toronto and a Scientist at the Toronto General Hospital Research Institute within the University Health Network (UHN) in September 2018. Her expertise is in human immunology, immune tolerance and immunotherapy. Dr. Crome’s research is focused on uncovering cells and molecules that regulate immune tolerance, and identifying underlying causes of transplant rejection. Her translational research as part of the Multi Organ Transplant Program at UHN involves the identification of novel immunotherapeutic targets and development of cell-based therapies for transplantation and autoimmunity.
Dr Crome’s scientific career started at the University of British Columbia with Dr. Megan Levings, where her research defined molecular, epigenetic and cellular regulatory mechanism that control human CD4+ T helper 17 cell development and their pro-inflammatory functions. Her postdoctoral work with Dr. Pamela Ohashi at Princess Margaret Cancer Centre discovered a novel innate lymphoid cell (ILC) population that inhibits the activity and expansion of tumour-associated T cells and is associated with poorer clinical outcomes in ovarian cancer. Dr. Crome holds the Next Generation of Scientists award from the Cancer Research Society and is a Medicine By Design Investigator.
Contact: email: sarah.crome[at]utoronto.ca twitter: @sarah_crome phone: 416.634.8097 address: 2-805 PMCRT | 101 College St | Toronto ON M5G 1L7 | Canada
Websites with additional information: https://www.immunology.utoronto.ca/faculty/sarah-crome https://www.uhnresearch.ca/researcher/sarah-q-crome
Current Lab Members:
Graduate Students
Kyle Reid (PhD Student) Julia Murphy (PhD Student)
Sarah Colpitts, MSc (PhD Student)
Sinthuja Jegatheeswaran, MSc (PhD Student)
Martin Mak (PhD Student)
Johanne Audouze (MSc Student)
Sia Mashhouri (PhD Student)
David Luong (PhD Student, co-supervised)
Undergraduate Students Ana Sofia Mendoza Viruega
Wenhui Cui
Staff Jessica Mathews, MSc
Humaira Murshed
Nadia Sachewsky, PhD (Microsurgeon)
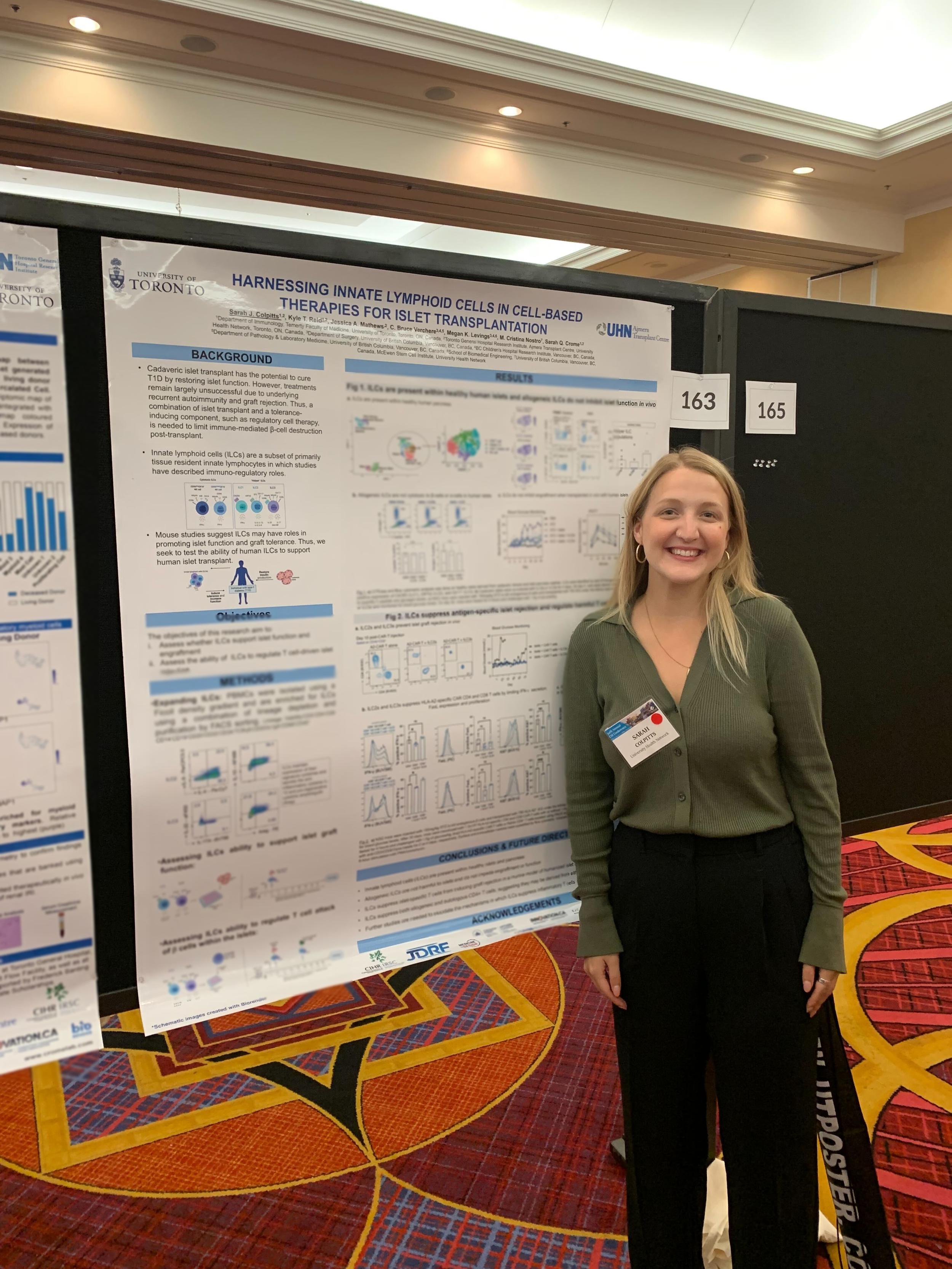
Sarah Colpitts
Sarah is a characterizing the role of innate lymphoid cells in type 1 diabetes (T1D). T1D is an autoimmune disease in which inflammatory CD4+ T cells mediate attack against pancreatic islet β-cells, which secrete insulin and facilitate the break-down of glucose. I am exploring how the tissue regenerative and regulatory properties of ILCs influence effectiveness of islet transplantation, and how ILCs are altered in T1D.
Jessica Mathews
Jessica is investigating the role of cytokines on the development and function of ILC subsets. Understanding the impact of cytokines are key for harnessing ILCs in novel therapies
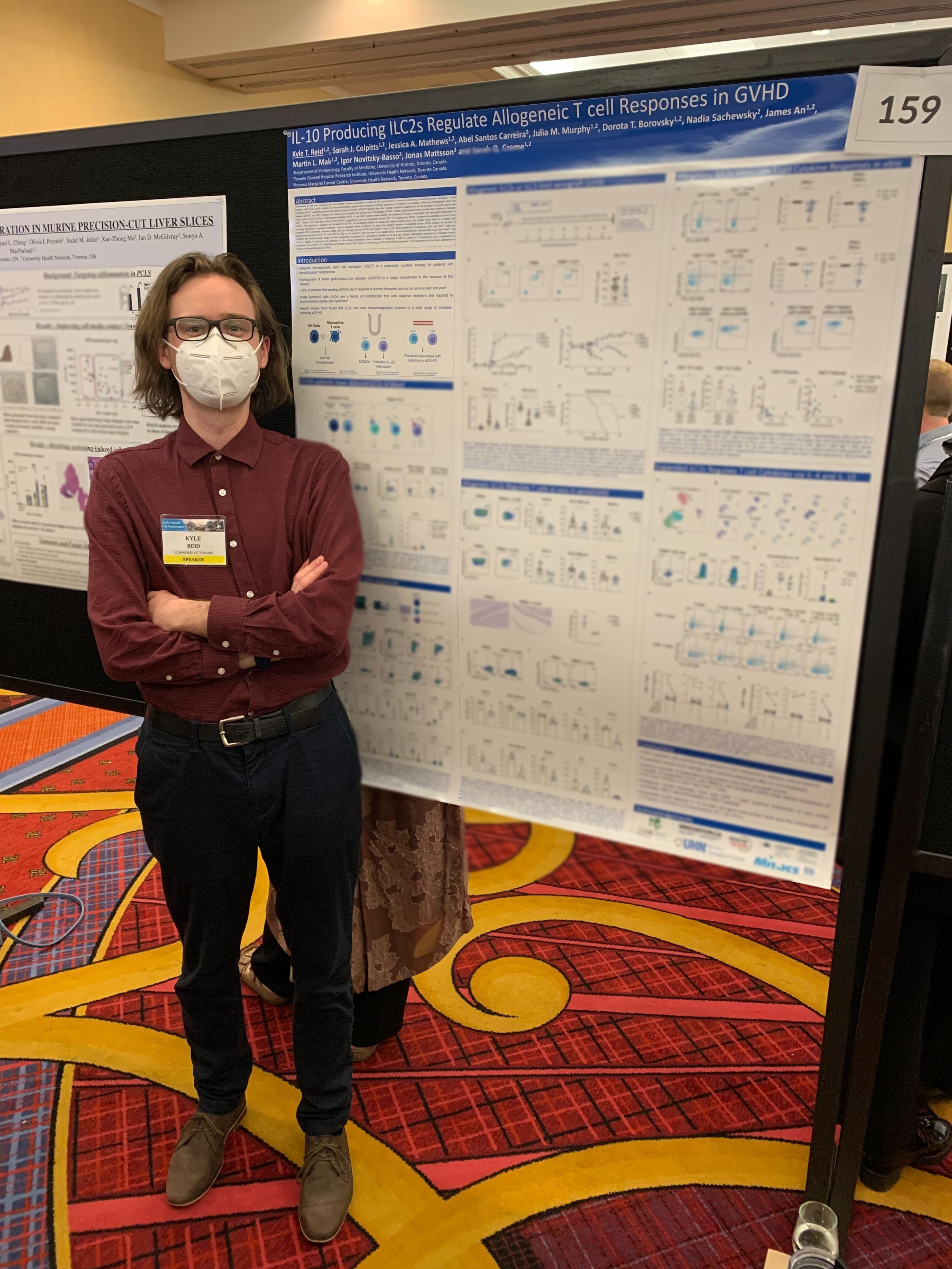
KYLE REID
Development of graft-versus-host disease (GVHD) is the primary factor limiting the success of hematopoietic stem cell transplant (HSCT) in treating hematological malignancies. Kyle is focused on determining if and how different ILC subsets contribute to protection from the development of GVHD. He is combining single cell RNA sequencing of patients undergoing HSCT, humanized mouse models of GVHD and advanced immunological platforms to understand ILC interactions that are protective in these contexts.
JULIA Murphy
Julia is investigating the role of human innate lymphoid cells (ILCs) and other tissue-resident immune cells in kidney transplantation. She harnesses multi-omic single-cell approaches and functional assays to identify and characterize ILCs in kidney from healthy living donors and transplant recipients to identify immune cells and pathways that impact clinical outcomes in kidney transplant recipients.
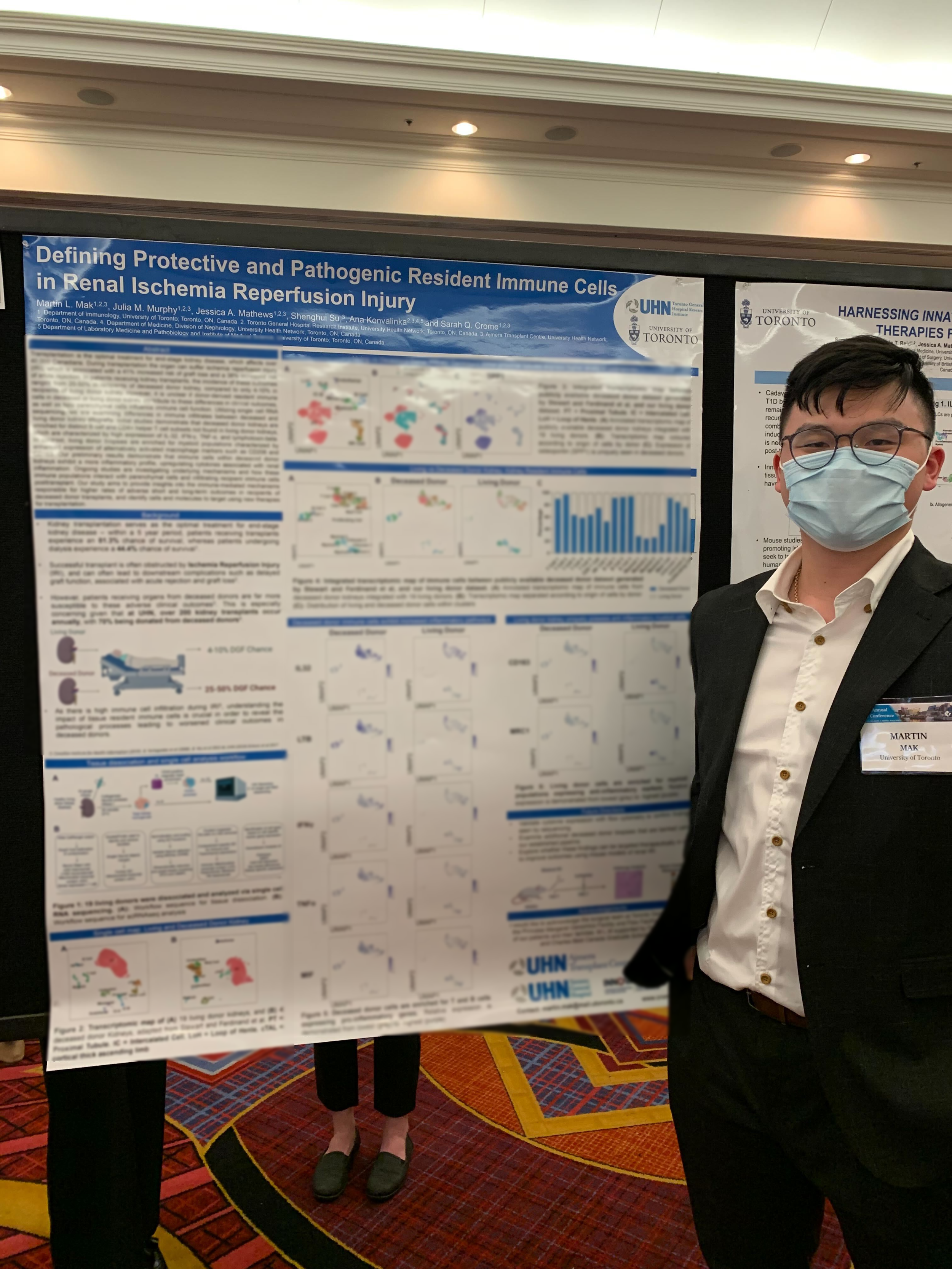
MARTIN MAK
Martin is focusing on the role of tissue resident immune cells in kidney transplantation, with the aim of determining what causes recipients of deceased kidney allografts to exhibit worse clinical outcomes than recipients of living kidney allografts. Martin makes use of multi-omic single cell techniques to focus on immune cell differences between living and deceased donor kidneys, which will be combined with our cell and tissue culture models to reveal host and donor immune differences.
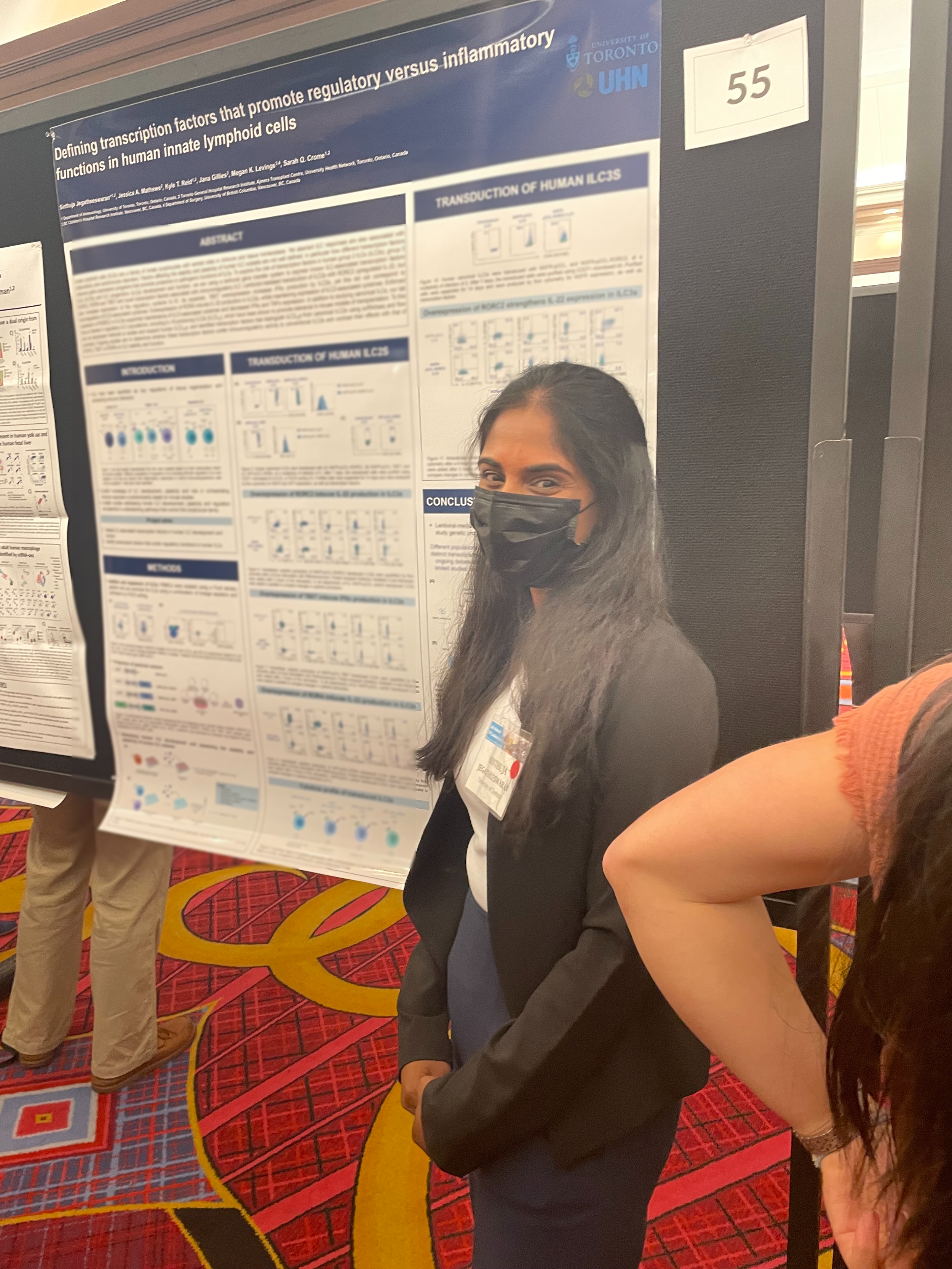
SINTHUJA JEGATHEESWARAN
Sinthuja is investigating the interaction between human innate lymphoid cells (ILCs) and regulatory T cells (Tregs), and its cell therapy potential in the context of type 1 diabetes (T1D) and islet transplantation. She is exploring the ability of ILCs, in combination with Tregs, to promote tolerance and function of transplanted beta-like cells. She will also harness lentiviral vector-based systems to investigate the role of ILC associated transcription factors on human ILC development and function, and explore the potential of different transcription factors to confer immunoregulatory function of ILCs.
Johanne Audouze
Johanne is optimizing the use of Crispr-Cas9 technology in innate lymphoid cells (ILCs). She is also investigating the effects of Crispr-Cas9 mediated knockout of cytokine genes and transcription factors on ILC’s phenotype and function. Understanding further the function of these genes in immune tolerance is important to help developing new therapies involving ILCs in the context of transplantation.
Alumni:
James An, MSc
Dorota Borovsky, MSc
Sofija Bekarovska, MSc